Gut issue biomarkers and their use in signalling dysbiosis
/Article by Jackie Zions
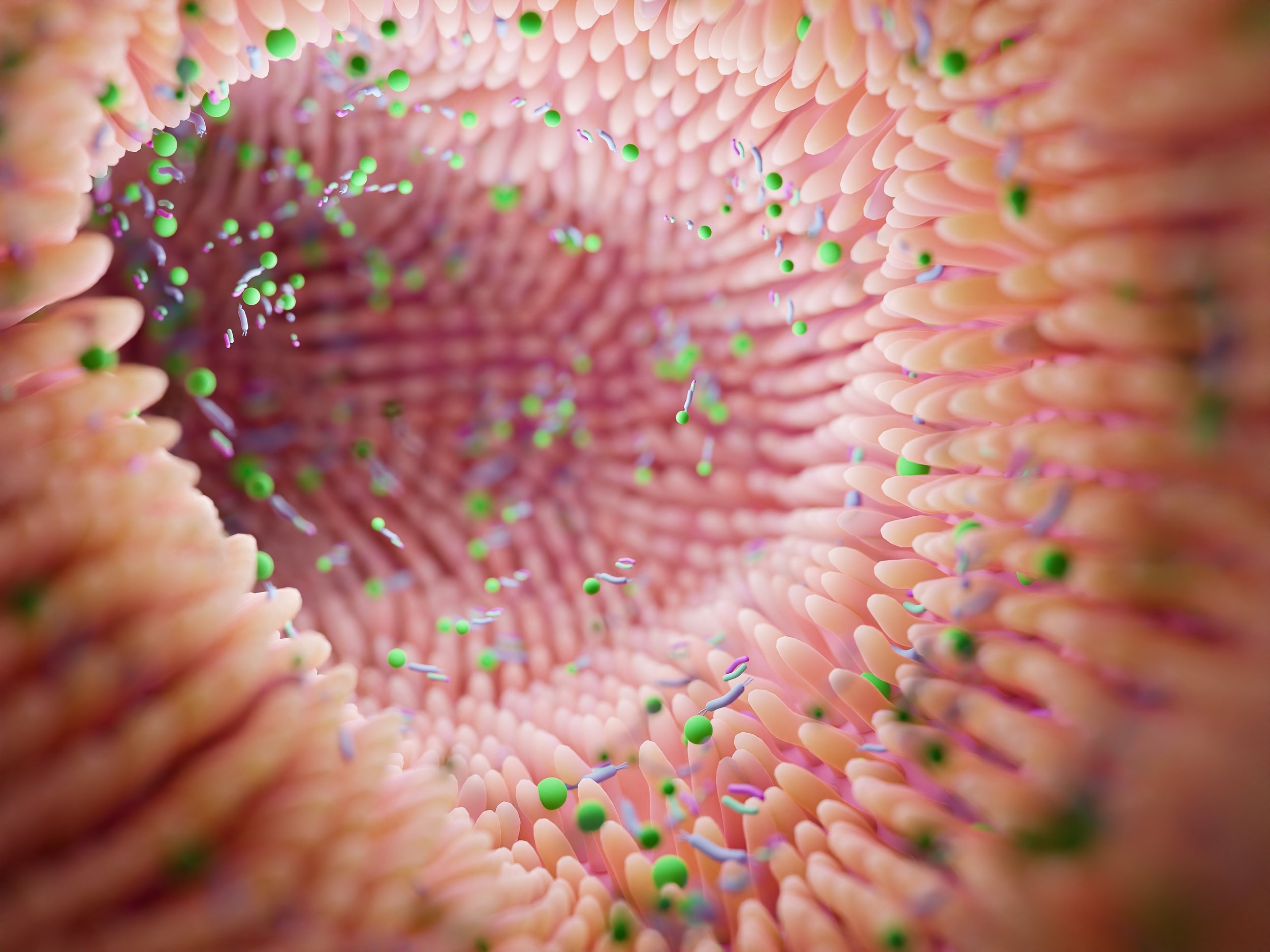
Gastrointestinal issues (GI) are the number one cause of morbidity in horses other than old age. An unhealthy digestive system can cause poor performance, pain, discomfort, diarrhoea, and a whole host of issues that can sideline your horse. It’s no wonder researchers are paying close attention to the ‘second brain’ and its billions of inhabitants. Ontario Veterinary College (OVC) researcher, Dr. Luis Arroyo has been studying the equine gastrointestinal systems for many years with several research projects receiving funding from Equine Guelph. Arroyo discusses what we know about equine gut health, causes of GI disorders and the extensive continuing research to understand what unstable and stable gut populations look like.
Starting with some basic anatomy Arroyo says, “The gastrointestinal tract of a horse is extremely large, and there are many things that can cause disturbances to the normal functioning or health of the gut.” A healthy gut microbiome is essential for the horse’s entire body to function optimally.
Signs of GI issues
Common signs of disorders could include abdominal pain, bloating, changes in faecal consistency (including diarrhoea or constipation), excessive drooling, decrease in water consumption, lack of or poor appetite, weight loss and low body condition score.
“Some cases are more obvious to owners,” says Arroyo, “like poor performance, or acute or chronic diarrhoea.”
Changes of behaviour such as becoming cranky or moody can be tell-tale signs there is unrest in the GI system. Biting at the flanks can signal abdominal pain as well as reactivity to being saddled. When the horse stops wanting to perform and athletic abilities suddenly decline, if there is no obvious lameness, GI issues are high among the considerations.
“Horses are herbivores, designed to consume a diet of forage, and to break down complex sugars within that forage.” says Arroyo. “The gut microbiota does this job and is very important for healthy digestion.” Recent research is connecting the changes in diversity of microbial communities to conditions like colic, colitis, and gastric ulcers.
Causes of GI Issues
Colic is the number one clinical condition occurring in horses. It is well-known that sudden dietary changes can be a major contributor as well as diets that are high in grain. This can create changes in the volatile fatty acids produced in the GI system, which in turn can lead to the development of gas colic. Arroyo provides the example of switching from dry hay fed in the winter, to rich, lush, spring grass as a big cause of rapid fermentation that can cause colic.
Any abrupt change, even if it’s a good quality feed to a different good quality feed, can be a source of colic. Then there is the more obvious consumption of mouldy, poor quality hay. So not only the quality but the transition/adaptation period needs to be considered when making feed changes and this goes for both changes to forage or concentrates.
A table of feed transition periods on the Equine Guelph website states an adaptation period of at least 10 – 14 days is recommended. Transition periods under seven days can increase colic risk over 22 times! (https://www.equineguelph.ca/pdf/tools/How%20to%20Transition%20Feedstuff.pdf)
“Decrease in water consumption can be an issue, especially in countries with seasons,” says Arroyo. When water gets really cold, horses often drink less, and if it freezes, they don’t drink at all, which can lead to impaction colic. Parasite burden can also cause colic. If your horse lives in a sandy environment, like California, ingesting sand can cause impaction colic.
Non-steroidal anti-inflammatory drugs (NSAIDS) can cause colic or ulcers. NSAIDS can interfere with blood supply to the GI tract causing ulceration, for example in the mucosa of the stomach. Prolonged use can cause quite severe ulceration.
NSAIDS are not the only drugs that can contribute to GI issues. “Antibiotics - as the name says - kill many kinds of bacteria,” says Arroyo. “They are designed for that! Invariably they deplete some bacterial populations including in the intestine, and that is a problem because that may allow some other bacteria, potentially pathogenic or harmful, to overgrow, and that can cause dysbiosis.”
In a recent study, by fellow OVC researcher, Dr. Gomez and co-workers, it was determined that damage to the intestinal microbiota could occur after only 5 days of administering antibiotics to horses. Damage to the intestinal microbiota resembled dysbiosis that can potentially result in intestinal inflammation and colitis predisposing the horse to diarrhoea. Judicious use of antibiotics and antimicrobials are advised.
There are infectious and non-infectious causes of colitis. Infectious examples include salmonella and then there is Neorickettsia risticii, which if ingested from contaminated sources, can cause Salmonellosis or Potomac horse fever, respectively.
“Any stress factors such as transportation, fasting or intense exercise like racing, can be a factor for developing stomach ulcers,” says Arroyo.
Current Diagnostics
Putting together a picture of the horse’s health status includes gathering clinical history from the horse owner and performing a physical examination for motility and hydration status. A biochemistry profile and complete set count can be gathered from blood testing.
Gastric ultrasound allows veterinarians to view the wall of the intestine, noting if it has thickened or distended, which could occur in cases when there is colic. They can assess appearance and find out if the intestine is displaced or if there is a twist. Gastroscopy is commonly used to find ulcers in the stomach and can reach as far as the first part of the duodenum.
GI Research
“DNA sequencing has been a breakthrough in science in terms of understanding the communities of different microorganisms living in many different niches from the skin to the lungs to the upper airways to the intestine,” says Arroyo.
It has allowed in-depth study of the population of microorganisms, providing a big picture of the different inhabitants in various areas of the GI tract, such as the lumen of the small intestine and the small and large colon. “The microorganisms vary, and they have different functions in each compartment,” says Arroyo.
DNA sequencing has allowed researchers to study microbial populations and gather information on what happens to bacterial communities when impacted by diseases like colitis. “We can see who is down, and who is up,” explains Arroyo, “and determine what populations have been depleted.” It has led to a better knowledge of which of the billions of factors are harmful to the system and which can compromise the health of the horse.
Robo-gut is one example of a fantastic system where bacterial communities are being replicated in the lab to mimic what would be found in a natural environment.
Researchers at the University of Guelph have measured metabolic profiles of the bacterial population after the addition of supplements like probiotics and prebiotics. They found they can dramatically change the metabolites that are being produced, according to what is being added to the system.
Exciting new research that could impact the future of diagnostics includes screening for biomarkers as indicators of intestinal health among equine microbiota. Dr. Arroyo is currently working with research partner, Dr. Marcio Costa, from the University of Montreal, looking for biomarkers that indicate changes in the inhabitants of the equine gut that take place during the early onset of illness.
“A biomarker is a biological molecule that you can find in different places,” explains Arroyo. “For example, you might find them in tissue, blood, urine, or different body fluids. They can signal normal or abnormal processes or could reveal a marker of a disease. For example, a biomarker can be used to see how well the body might respond to a treatment or to a disease condition.”
“The objective of a dysbiosis index is quantifying ‘X’ number of certain bacteria that are important to us,” says Arroyo. In this case, the dysbiosis derives from sequencing of the bacterial population in faecal samples.
Changes in the intestinal microbiota (dysbiosis) are present before and during the outset of diseases and after treatment with antibiotics. Arroyo cites the example of decreased Lachnospiraceae commonly observed when there is intestinal inflammation.
Bacterial biomarkers are currently being used in other species to accurately predict intestinal dysbiosis, for example in cats and dogs. One canine study quantified the number of seven different taxa of importance of the total bacterial populations. This information is entered into a mathematical algorithm that comes up with results explaining which bacteria have increased or decreased. Based on those numbers, one can use a more specific taxa to identify dysbiosis. In a feline study, it was discovered that six bacterial taxa could be accurately used to predict diarrhoea in 83% of cases.
It is hoped the same results could be accomplished for horses. Developing PCR testing to screen for biomarkers could be a game changer that could potentially provide speedy, economical early diagnostics and early treatment.
So far, the most remarkable finding in the preliminary data reveals that in horses with colitis, the whole bacterial population is very depleted.
“At this stage we are in the process of increasing our numbers to find significant differences in which bacterial taxa are more important,” says Arroyo. “Soon we hope to share which bacteria taxa are more promising for predicting dysbiosis in horses with gastrointestinal disease.”
The researchers are delving into a huge biobank of samples to identify potential markers of intestinal dysbiosis in horses, utilising PCR testing as a faster and more economical alternative to the complex DNA sequencing technologies that have been used to characterise changes in microbiota thus far. The goal is to develop simple and reliable testing that veterinarians can take right to the barn that will result in early treatment and allow closer monitoring of horses at the first onset of GI disease.
Top Tips to Protect Digestive Health
Horses are hind gut fermenters who rely on adequate amounts of fibre in the diet to maintain healthy gut function.
Make dietary changes slowly as abrupt changes disrupt the microbiota.
Avoid large grain meals as huge portions of highly fermentable diets can be quite harmful to the microbiota and can also be a source of risk for developing gastric ulcers. Opt to spread out concentrates into several smaller rations.
Prevent long periods of fasting which can also lead to ulcers. Horses are continuous-grazers, and they need to have small amounts of feed working through their digestive system to keep it functioning optimally.
Have a parasite prevention programme.
Provide fresh water 24/7 to maintain good hydration and keep contents moving smoothly through the GI tract.
Keep up to date on dental appointments.
Motion is lotion – turn out and exercise are extremely important to gut function.
In closing, Arroyo states, “These top tips will help keep the horse happy and the gastrointestinal tract functioning properly.”